Ovarian Cysts
Because ovaries are in the “business” of cyst-making, not every mass that develops is dangerous. Each month a woman forms a cyst in preparation to ovulate (releasing an egg) after egg release, another cyst forms called a corpus luteum. Either cyst may become larger or more painful than usual. Sometimes a cyst will disrupt blood vessels and cause bleeding into the abdomen or into the cyst itself. Either situation may be quite painful. If a cyst becomes larger than about 2 inches in diameter it may twist on its stalk and cut off its own blood supply causing severe pain. Ultrasound, observation, and, in postmenopausal women, a special blood test, can help distinguish between benign (safe) and potentially malignant (very dangerous) masses
 Few cysts present with sudden pain
Few cysts present with sudden pain
Unless they are twisting (undergoing torsion), are bleeding or are in the process of rupturing … cysts do not usually cause severe pain. About 8% of women (with no symptoms) between the ages of 25 and 40 have ovarian cysts larger than 2.5 cm. Although many cysts resolve spontaneously, some women may be subjected to unnecessary surgery because of concerns about ovarian cancer. In actuality, various studies have shown that cysts found prior to menopause are benign in 87% to 93% of women, and cysts found after menopause are benign in 55% to 92% of cases. The gynecologist’s dilemma is to differentiate between cysts that require surgery and those that do not.
Untwisting of the twisted ovary restores function
When the ovary has twisted and cut off its own blood supply, rather than resort to removal of the ovary, It may be simply untwisted. Studies have shown that this maneuver leads to a return of normal ovarian function. In addition, no case of thromboembolism (blood clot) has ever been reported following the detorsion of an adnexa.
Physical clues to the type of cyst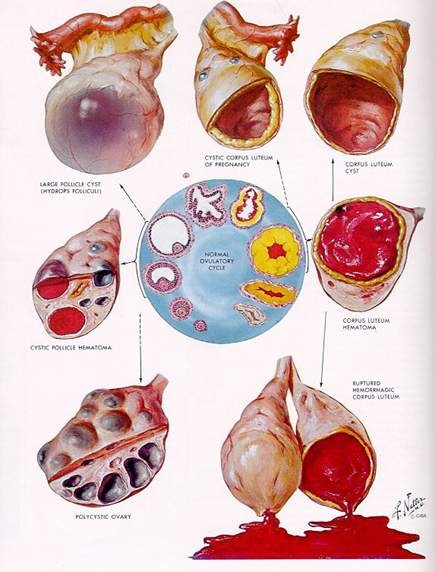
The pelvic examination can yield important clues. For example, a mass that is soft, smooth, and freely mobile is likely to be benign. Tenderness is more common with a hemorrhagic cyst or with torsion and is rarely associated with cancer. A solid, fixed, irregular mass, however, should raise the suspicion of cancer. If ascites or an abdominal mass is found, then a full careful evaluation to rule out danger is necessary.
Ultrasound appearance
It is extremely important for the Gynecologist to either do an ultrasound or personally view the actual images. The reason: Many radiologists use the term “complex” to describe all cysts other than totally clear, simple cysts. However, many benign ovarian changes are complex, such as dermoid cysts, endometriomas, hemorrhagic cysts, and cystadenomas. A careful review of the images and, at times, other imaging studies, can help determine the most likely diagnosis.
Some ovarian cysts (Dermoids) can often be confirmed by limited computed tomography scan (CAT Scan) when fat (sebaceous material), teeth, or bone are seen within the ovary.
Torsion may be suspected when a test called Doppler imaging shows decreased or absent blood flow to the ovary.
A small amount of free fluid in the pelvis is an indication of possible cyst rupture. If a hemorrhagic cyst is present, a follow-up ultrasound about 2 weeks later may show either a smaller cyst or changes in the internal echoes consistent with an organizing clot.
False-positive Blood Tests
Blood test markers such as CA 125 or OVA1 are rarely helpful in determining how to manage a cyst in a young woman and should be avoided in the premenopausal population. Abnormally high CA-125 values can occur with endometriosis, functional cysts, fibroids or adenomyosis, pelvic infection, pregnancy, and cyclic elevations associated with the menses. In a premenopausal woman, the chance of a false-positive CA-125 reading is about 70% whereas 50% of women with stage I ovarian cancer have a negative ca125 test.
2 useful markers
Very young women are at risk for developing germ-cell tumors and may benefit from β human chorionic gonadotropin or alpha-fetoprotein blood tests. Thus, these tumor markers are sometimes helpful in this patient population.
Management options
In many cases, the first option should be observation and a repeat ultrasound in about 2 weeks. Pain medications and rest can be helpful to control pain. Reassure her that the pain should diminish in a few days, although it sometimes takes longer.
Skip the birth control pills
Even with simple cysts presumed to be normal, birth control pills do not help them go away faster.
Pain may warrant surgery
In rare cases, a woman may have such severe pain that rest and analgesics are ineffective, and surgery is warranted for pain alone. In other cases, a cyst that appears functional or hemorrhagic on sonography but persists more than 8 weeks may justify removal to rule out neoplasia.
In a premenopausal woman with a probably benign ovarian cyst who requires surgery for pain or because the cyst fails to resolve, surgery can usually save the ovary, if at all possible. Even with a large cyst (6 cm or larger), saving the ovary is possible. Laparoscopic surgery, which involves a short hospital stay and faster postoperative recovery, should be considered unless a dangerous tumor is suspected.
Postmenopausal women
Many menopausal women with ovarian cysts worry that they might have ovarian cancer. Even if no symptoms are present. Most cysts are benign, observation and repeat sonograms are usually justified unless the ultrasound appearance is worrisome or worsening symptoms are present.
About 6% of Postmenopausal women have small (less than 5 cm) cysts when they are carefully screened with ultrasound. A study of 15,106 women age 50 or older found 2,763 (18%) had simple cysts less than 10 cm in size on ultrasound exam. Seventy percent of the women had the cyst go away within 6 weeks, and none of the 220 women with persistent simple cysts developed ovarian cancer after an average follow-up of 6.8 years. In properly selected patients, risk of cancer was close to zero.
Conclusions:
Simple cysts are nearly always benign.
Ovarian cancer is almost always associated with complex ovarian cysts.